Total Hip Replacement
Dr. Brian Grisez’s Total Hip Replacement
Whether you are just beginning to explore treatment options, or have been directed here by your physician, this page will help you be better informed concerning total hip replacements.
The first total hip replacements were performed in the 1960’s. Since then, great strides in implant technology and surgical technique have improved the success of the surgery. Today it is recognized as one of the most valued developments in orthopaedic history. For patients with debilitating pain from a diseased hip joint due to arthritis and other causes, total hip replacement can be an excellent option to restore function and mobility.
ANATOMY OF THE HIP
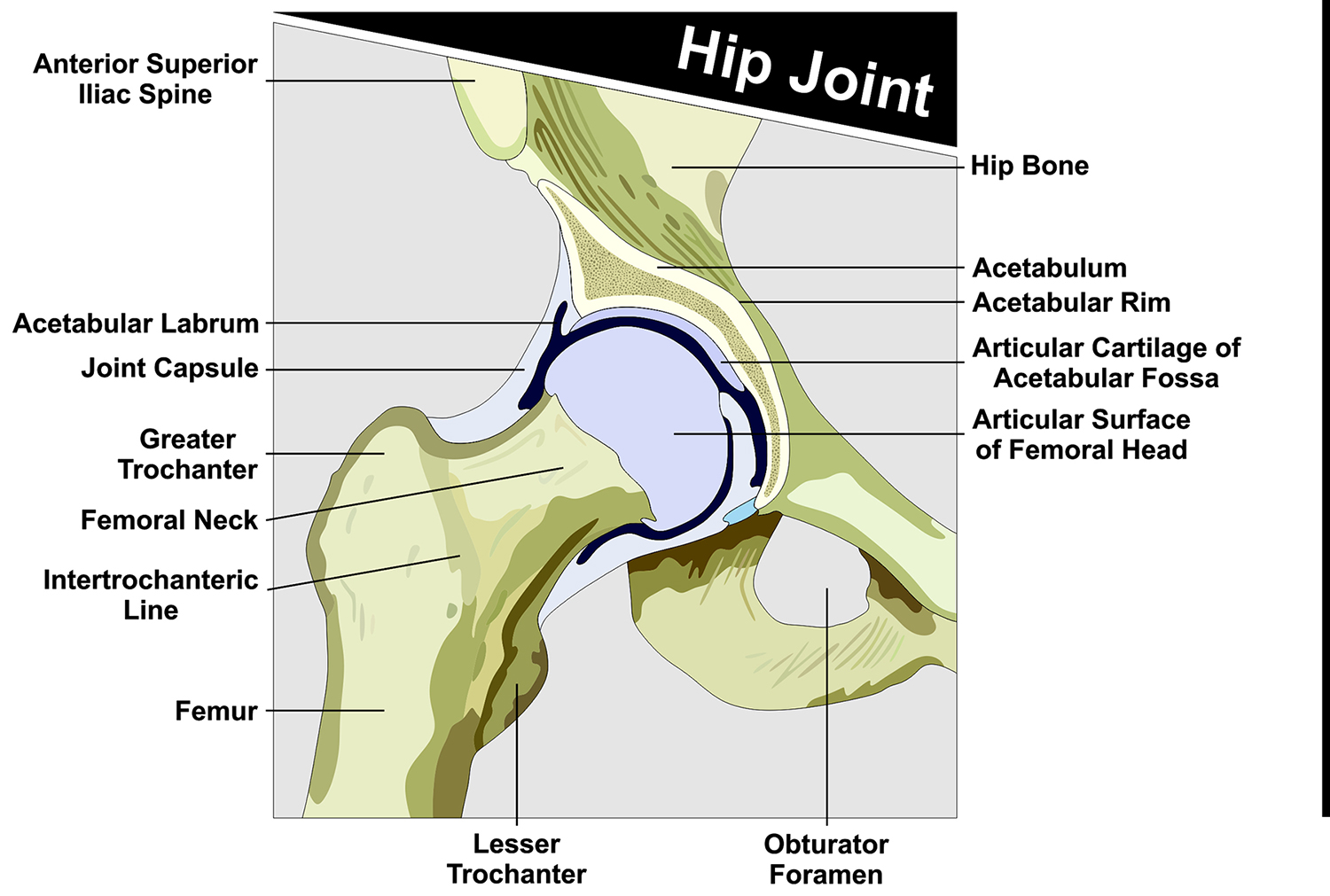 The hip is a large joint composed of a ball-and-socket. The “socket” portion of the hip is part of the acetabulum (large pelvis bone) while the “ball” is the femoral head (upper end of the femur (thighbone)). Both the ball and socket portion of the joint are covered with articular cartilage, a smooth tissue that cushions the ends of the bones and enables them to move easily.
The hip is a large joint composed of a ball-and-socket. The “socket” portion of the hip is part of the acetabulum (large pelvis bone) while the “ball” is the femoral head (upper end of the femur (thighbone)). Both the ball and socket portion of the joint are covered with articular cartilage, a smooth tissue that cushions the ends of the bones and enables them to move easily.
In a healthy hip, the membrane that surrounds the hip joint makes a small amount of fluid that lubricates the cartilage and eliminates almost all friction during hip movement.
Bands of tissue called ligaments (the hip capsule) connect the ball to the socket and provide stability to the joint.
COMMON CAUSES OF HIP PAIN
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
- Osteoarthritis. Sometimes called degenerative joint disease or degenerative arthritis, osteoarthritis (OA) is the most common chronic condition of the joints, usually occurring in people 50 years of age and older. OA causes the smooth cartilage areas to wear away allowing the bones to rub against each other, causing hip pain and stiffness.
- Rheumatoid arthritis. With this disease, the body’s immune system attacks its own tissue, including joints. Rheumatoid Arthritis (RA) affects joint linings, causing painful swelling and damage. Over long periods of time, the inflammation associated with rheumatoid arthritis can cause bone erosion and joint deformity.
- Post-traumatic arthritis. This can follow a serious hip injury or fracture. The cartilage may become damaged and lead to hip pain and stiffness over time.
- Avascular necrosis. Also called osteonecrosis or bone infarction, is death of bone tissue due to interruption of the blood supply. Early on there may be no symptoms. Gradually joint pain may develop which may limit the ability to move.
- Childhood hip disease (Hip Dysplasia). Some infants and children have hip problems. Even though the problems are successfully treated during childhood, they may still cause arthritis later on in life.
DESCRIPTION OF THE TOTAL HIP REPLACEMENT PROCEDURE

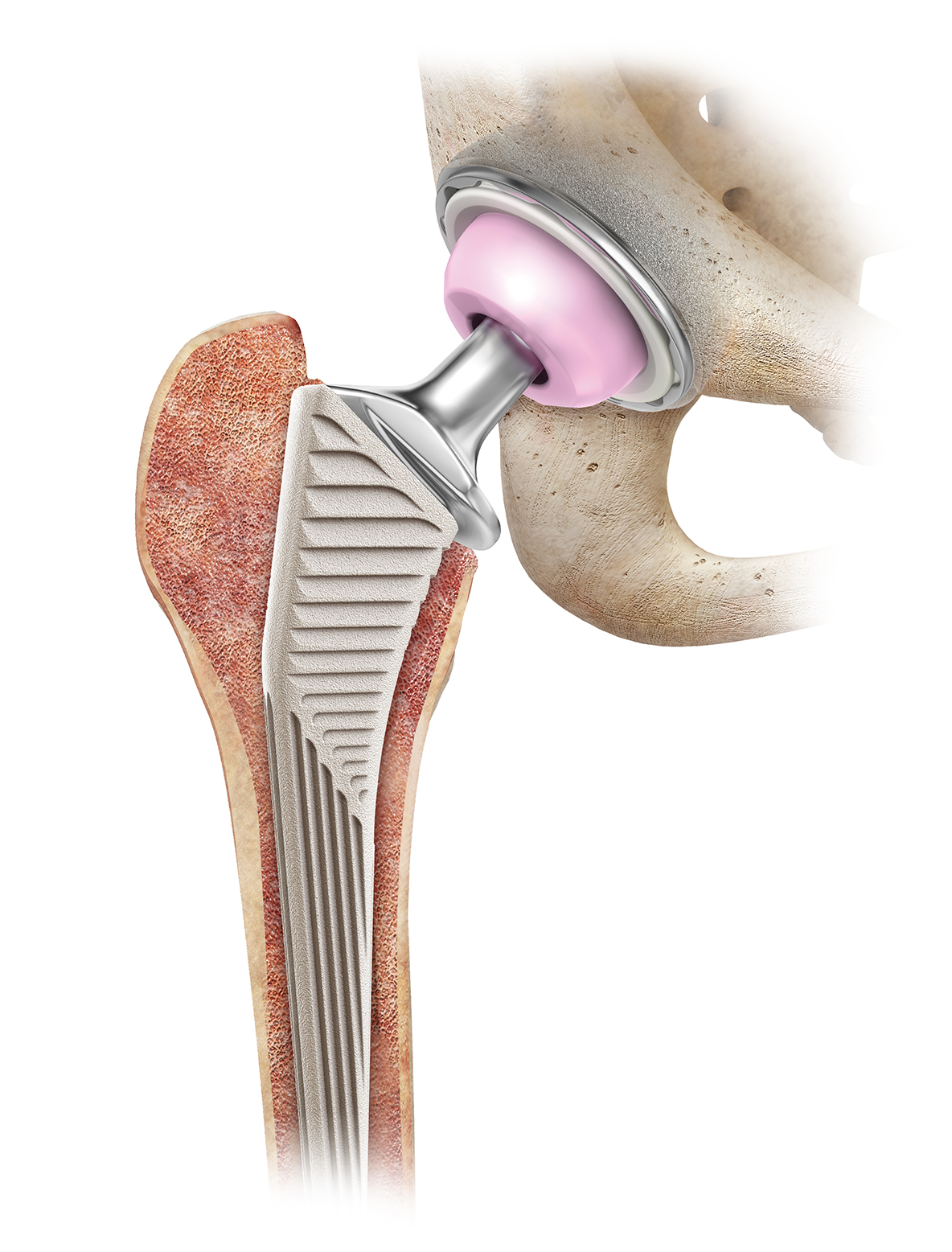
An incision is made on the front of the hip (more below on the Anterior Approach to Hip Replacement) to access the hip joint. The damaged femoral head (ball) is cut and removed. Any remaining cartilage within the socket (acetabulum) is also removed. A metal shell is then placed in the acetabulum. A liner, most often made of strong plastic is inserted and locked into the metal shell. An individually sized metal stem made of titanium is placed into the femur. A metal or ceramic ball is then placed on the upper part of the stem. This adjoining with the plastic liner creates the new hip joint. Over time, your bone will incorporate into the metal shell and stem to give long term fixation.
TOTAL HIP REPLACEMENT BY BRIAN T. GRISEZ, MD
Brian T. Grisez, MD specializes in all approaches to hip replacement. During surgery the hip can be accessed through the front – the anterior approach, the side – lateral or anterolateral approach, or the back – posterior approach. Each has its own advantages and disadvantages. For first time hip replacements (and even many revisions), my preferred approach is through the front of the hip or the direct anterior approach. This is not a new approach but has gained popularity in recent years as our knowledge of the anatomy and technical nuances of the surgery have been refined. By accessing the hip from the front, the muscles and tendon attachments are separated and not cut. In most patients, this results in less post-operative pain, shorter hospital stays, lower dislocation rates, and a swifter earlier recovery.
During the surgery, Dr. Grisez utilizes fluoroscopy (live x-ray) to assess implant sizing and positioning as well as limb length. All patients are up and walking on the day of surgery and many go home the same day. The need for “hip precautions” is usually not necessary as well. The decision of which approach is individualized and discussed at the patient’s pre-operative appointment.
THE TOTAL HIP REPLACEMENT – SURGICAL PROCESS EXPLAINED:
- Diabetics – Make sure your blood sugar control is extremely good in the weeks prior to your procedure. We will check your levels the morning prior to surgery and it must be less than 120. If not, your surgery will likely be postponed.
- Nicotine – If you use any form of nicotine, we ask that you stop for 6 weeks prior to your surgery and continue not to use after surgery as this will help with the healing process. This includes all forms of nicotine – smoking vaping, dip, chew, etc. Infections and wound complications after joint replacement surgery are disastrous and unnecessary risk factors.
 Obesity – Being severely over weight can impact your healing negatively. We require that surgical patients have a BMI score of no more than 35 (Click here for additional information on body mass index and the weight loss diet).
Obesity – Being severely over weight can impact your healing negatively. We require that surgical patients have a BMI score of no more than 35 (Click here for additional information on body mass index and the weight loss diet).- Nourishment – It is vital that you take care of yourself and eat a healthy diet consisting of plenty of vegetables (green and other colored) and proteins (eggs, bacon, beef, pork, poultry, fish (no batter please). Cut out all unnecessary sugars and starches (the “white stuff” such as bread, rice, grits, potatoes, corn, chips, sodas and junk food in general). Try to eat well-balanced meals to give your body the nutrition it needs to heal.
- Skin – It is important to take care of your skin in the weeks prior to surgery! No bug bites, scratches, infected lacerations, etc – these allow additional places for germs to hide.
- Dental – Make sure your dental health is good – no abscessed teeth/infections, etc.
- Toe & Fingernail health – This must be excellent. No draining, bleeding, inflamed, infected or ingrown nails.
- Narcotic Pain Medications – Discontinue these medications if at all possible.
PLAN FOR YOUR SURGERY: BEFORE AND AFTER!
Make sure to plan on the fact that you are having surgery.
- Designate a close friend or family member as your “Patient Champion”
- As a patient champion, this person will be responsible to help you throughout the process of your surgery. Your patient champion will have the following responsibilities:
- Attend your Pre-Op appointment with you.
- Bring you to the facility on the day of surgery.
- Drive you home and help you into your residence.
- As a patient champion, this person will be responsible to help you throughout the process of your surgery. Your patient champion will have the following responsibilities:
- Make sure you have friends and family lined up to help you during the healing process.
- Make sure there are no trip hazards at your home.
- You will be given a prescription for pain medications after surgery – make sure someone can get it for you.
- Become an active member in your recovery process.
- You can do this! Your determination to succeed is critical!
STEP 2 Getting Started – Final Office Visit With Dr. Grisez
- Patient Champion – Make sure to bring your patient champion with you if at all possible.
- Templating / Sizing X-Rays – We will take general x-rays of your hip and using specialized software, develop exact sizing for the replacement joint.
- Laboratory Screen – Blood work will be drawn or reviewed.
- Surgical Clearance – If needed, we will obtain or review surgical clearance from your current primary care physician and/or specialist (cardiologist, pulmonologist, neurologist, etc).
- Questions – Final questions and plans discussed with Dr. Grisez.
STEP 3 Pre-Op Packet Pick-Up From BJISG
Patients will come by BJISG at an appointed time and pick up their completed Total Joint Packet which will include the following:
- Post-Op Pain Medication Narcotic Agreement
- Post-Op Prescriptions
- DME Prescription
- Diabetic Pre-Op Instructions (for diabetics)
- Discharge Instructions
- Surgery Check follow-up appointment
- Total Hip Replacement Brochure
STEP 4 Pre-Op Appointment
Your pre-op appointment will be held at the surgical facility.
- Patient Champion – Make sure to bring your patient champion with you if at all possible.
- Pre-Surgery Testing – Additional blood will be drawn for labs and an EKG will be taken.
- Final Surgery Consult – final details will be discussed prior to surgery. We will explain what and when to stop taking medications at this point and which need to be continued.
- Prescription Drugs – Discontinuing prescriptions that “thin” the blood as directed by your physician(s), such as aspirin is necessary prior to surgery. Any Narcotic/Opioid medications must be stopped prior to surgery as well.
- Food/Drink – Patients must refrain from eating or drinking as directed at the pre-op appointment. Make sure that you are well nourished and hydrated in the days and weeks prior to surgery (Water, Gatorade, etc).
STEP 5 Day Of Surgery
Here is what to expect the day of your surgery:
 Arrive at the surgical facility at the appointed time (with your patient champion).
Arrive at the surgical facility at the appointed time (with your patient champion).- Final pre-surgery assessment of vital signs and general health
- Diabetics – blood sugar checked and must be below 120.
- Meet with anesthesiologist and operating room nurse.
- Start IV (intravenous) catheter for administration of fluids and antibiotics.
- Dr. Grisez will see you, answer any last questions and “sign your surgical site”.
- Joint replacement surgery.
- Recovery room.
- Ongoing monitoring of vital signs until condition is stabilized.
- Diet of clear liquids or soft foods, as tolerated.
- Physical therapist helps you to your feet to stand and walk.
- Begin post-op activities taught during pre-op visit.
STEP 6 Going Home – Same Day / Next Day
Typically, patients who undergo Total Hip Arthroplasty may require a 1-2 night hospital stay but some patients can go home the same day as their surgery. Each patient recovers differently but all must reach the following goals before being discharged home:
- Vital signs stable (Blood pressure, heart rate, temperature, respiration)

- Ability to get from the bed to the bathroom and back to the bed with or without a walker.
- Ability to walk 50 feet down the hall and back.
- Ability to urinate and have a bowel movement.
- Nausea and/or vomiting controlled.
- No medication interactions or adverse side effects.
- Ability to tolerate eating and drinking.
- Pain reasonably controlled with Oral Medications.
- Diabetic patients must have their blood sugars well controlled.
If you are released the same day, your patient champion will drive you home and help you into your house.
STEP 7 WALK – WALK – WALK!
![]() Your new hip joint can take your full body weight immediately. As soon as possible, walk! Walk with the assistance of a therapist, a walker, cane or fully independent – walking is walking and it helps the healing process! The more you walk, the better the circulation in your legs and hip joint – the better the healing.
Your new hip joint can take your full body weight immediately. As soon as possible, walk! Walk with the assistance of a therapist, a walker, cane or fully independent – walking is walking and it helps the healing process! The more you walk, the better the circulation in your legs and hip joint – the better the healing.
DR. GRISEZ WILL SEE YOU AT YOUR TWO WEEK APPOINTMENT AND THEN IT’S OFF TO THE RACES!
FREQUENTLY ASKED QUESTIONS – Click Any Question Below For The Answer!
Are there specific instructions for care after surgery?
Yes. We have prepared a document with instructions for your specific care after a total hip replacement.
These instructions cover very important subjects such as:
- ACTIVITY
- PAIN MANAGEMENT
- MEDICATIONS
- WOUND and DRESSING CARE
- SHOWERING
- COMPRESSION STOCKINGS
- COLD THERAPY
- SKIN & NOSE CARE
- DIET
- FOLLOW-UP APPOINTMENT
- WHEN TO CALL THE DOCTOR
- AT-HOME EXERCISES
When can I go home after surgery?
Typically, patients who undergo Total Hip Arthroplasty may require a 1-2 night hospital stay but some patients can go home the same day as their surgery. Each patient recovers differently but all must reach the following goals before being discharged home:
- Vital signs stable (Blood pressure, heart rate, Temperature, Respirations)
- Ability to get from the bed to the bathroom and back to the bed with or without a walker.
- Ability to walk 50 feet down the hall and back.
- Ability to urinate.
- Nausea and/or vomiting controlled.
- No medication interactions or adverse side effects.
- Ability to tolerate eating and drinking.
- Pain reasonably controlled with Oral Medications.
- Diabetic patients must have their blood sugars well controlled.
Why do I need to lose weight for surgery?
Depending on your Body Mass Index (BMI), you may be told that you need to reduce your weight prior to surgery. People with a BMI score of over 35 can have a harder time healing and an increased risk of complications.
Here are some of the specific complications associated with obesity after joint replacement surgery:
- Infection
- Poor wound healing
- Difficulty breathing
- Blood clots
- Blood loss
- Pulmonary embolism (a blood clot in the lungs)
- Increased risk of hip dislocation
CLICK HERE TO FIND OUT WHAT YOUR BMI SCORE IS AND MORE INFORMATION ON THE SUBJECT.
What are potential complications of a total hip replacement?
In most circumstances, complications after total hip replacement are uncommon but inherent to the procedure. In all likelihood you will have a normal recovery without problems. However, potential risks do include infections of the joint replacement (which can happen at any time during the life of the replacement), wound healing complications, dislocation, leg length discrepancy, loosening of the implants, fractures (during surgery or after), wear of the plastic liner, numbness around the incision, excessive blood loss requiring transfusion. Medical complications are also infrequent but include blood clots in the legs or lungs, heart attacks and strokes. This is not meant to be an all-encompassing list.
Your surgeon and the entire surgical team have worked diligently to put together a program that significantly reduces the risk of complications. Over the last few years the complication rates have definitely been reduced but the potential for complications still exist and have not been completely eliminated.
Should I continue to see my surgeon after I’ve healed?
It is important to follow up with your surgeon after your joint replacement. In most cases, joint replacements last for many years.
The frequency of required follow up visits is dependent on many factors including the age of the patient, the demand levels placed on the joint, and the type of replacement. We will consider all these factors and tailor a follow-up schedule to meet your needs.
In general, seeing your surgeon every three to five years is recommended.
Will I need to take antibiotics prior to seeing a dentist or having other surgical procedures?
The American Academy of Orthopedic Surgery (AAOS) and American Dental Association (ADA) have generally recommended short-term antibiotics prior to dental procedures (one dose one hour prior to dental procedure) for patients who have had joint replacements. This recommendation continues for up to two years after your joint replacement.
Two or more years after the replacement, continued use of antibiotics prior to dental procedures is based on the discretion of the treating surgeon and the patient. Your surgeon will consider many factors including whether or not you are at increased risk of infection due to immune suppression (i.e. diabetic, transplant patients, and rheumatoid arthritis).
The use of prophylactic antibiotics prior to dental cleanings and other invasive procedures remains controversial. Most orthopaedic surgeons now recommend lifetime prophylaxis. Patients should discuss whether or not they need antibiotics prior to dental or other invasive procedures with their treating orthopedic surgeon.
Will my implant set off metal detectors at airports and courthouses?
Usually patients with joint replacements will set off metal detectors. This should not be of great concern. It is reasonable for you to inform the TSA screening agent at the airport that you have had a joint replacement; however, you will still require screening and will need to follow the directions of the screening agent. There are millions of individuals with joint replacements, and screening protocols recognize that people who have had joint replacements may set off detectors. Joint replacement documentation is not required.
Watch This Video and Learn More About Metal Detectors and your new New Joint!
What restrictions will I have after surgery?
I generally advise against extremes of positions in the early recovery period but place very few restrictions on my patients after hip replacement. Many go back to skiing, snowboarding, waterskiing, hiking, climbing, golf, yoga, pilates, mixed martial arts and many others. High impact activities such as long distance running are discouraged but not prohibited.
When can I return to work?
Returning to work is highly dependent on your general health, activity level and the physical demands of your job. If you have a sedentary job, such as computer work, you can expect to return to work in two to three weeks. If you have a more demanding job that requires lifting, walking, or travel, you may need up to three months for full recovery
When can I drive?
Depending on which leg… the right hip would obviously take a little longer to properly use the brake and gas pedals. All patients have to be off narcotics and no longer depending on a walker before they are able to drive on their own. Most patients are driving at four to six weeks after surgery, and sometimes sooner if the operative leg is the left leg.
When can I walk after surgery?
The same day! Most people are walking with the assistance of a walker on the day of surgery. Prompt walking has been shown to reduce the risk of a post-operative blood clots and is an important part of your recovery. Within the first month or two after surgery, you may walk using a cane or no walking aids depending on your progress. Despite the rapid progression to moving without assistance, it is typically not recommended that you return to aggressive/sporting activities until the third month after surgery.
When can I shower?
We used advanced water proof bandages so typically you may take a shower the next day after surgery.
Will I need Physical Therapy?
This is very patient dependant, but Hip replacement patients need very little formal physical therapy. We want to make sure you are careful walking with crutches and/or walker. The hip is structurally sound soon as the surgery is over and is ready to be walked on.
How long does it take to recover?
The majority of people who undergo total hip replacement are able to participate in a majority of their daily activities by six weeks. By three months, most people have regained much the endurance and strength lost around the time of surgery, and can participate in daily activities without restriction. However, people make gains for up to a year after their hip replacement. While daily activities have resumed, it is important to avoid high impact activities to give you the best long-term outcome with your hip.
How long will I stay at the hospital or surgical center?
It varies. Some patients will go home the same day while others may need to stay a couple of days. This is highly dependent upon your condition before surgery, your age, and medical problems which can influence your recovery. A safe discharge plan will be arranged for you by our orthopaedic team.
Will I need general anesthesia?
How big will my scar be?
Typically, the incision will be about 4 inches long but depending on the surgical needs – it is what is done underneath the skin that counts not the length of the incision! Your surgeon will make the incision as large as it needs to be in order to perform an excellent surgery.
After surgery, is recovery very painful?
You may have relatively mild pain following the procedure, or you may have a more difficult time than others. Everyone is unique and handles and perceives pain differently. Keep in mind that while pain management has greatly improved, a pain-free surgery is unlikely. You will want to take your pain medicines as directed by your surgeon and minimize the amount of narcotic/opioids taken.
How long will a new hip joint last?
Hip replacements do wear and can eventually wear out. Unfortunately, an artificial hip is not as durable as your own hip. Because the hip replacement implants are made of metal and plastic, these materials wear over time, similar to the rubber on your car tires.
Studies show that hip replacements can last more than 20 years. This is dependent on many factors. The activity level, weight and age of the patient can effect the longevity of the joint. One very large study found that 80% of hip replacements were functioning well after 15 years in the younger (less than 65) patients, and 94% of the older (over 65) patients.



