Spine Services
Spine Services At BJISG
At the Bone & Joint Institute of South Georgia, one of our goals is to improve the quality of life for people with issues of the spine. We offer comprehensive diagnosis and treatment options for all type of back & neck issues. Whether our patients’ treatments are conservative or surgical, we are dedicated to applying leading-edge technology, the latest techniques and the most effective therapy to help improve their mobility and lives.
Treatment Options
Our physicians develop a complete, individualized treatment plan for each patient incorporating their diagnosis, lifestyle and treatment goals. We work as a team to achieve the best possible outcome for our patients.
Conservative Treatment
Whenever possible, our physicians will explore nonsurgical treatments first. These treatments may include medication(s), physical therapy, and/or injections to improve the patient’s condition.
Surgical Treatment
For some problems, surgery is the best solution. The surgeons at the Bone & Joint Institute of South Georgia are highly skilled in the latest minimally invasive techniques that are associated with less postoperative pain and a faster recovery. In the hands of our experienced surgeons, the benefits of surgical treatment usually far outweigh the risks. Whatever the diagnosis is for our patients, our specialists are dedicated to restoring their function and relieving pain to the greatest degree possible by applying their knowledge and skill, combined with the latest techniques and advanced technology.
Minimally Invasive Endoscopic Spine Surgery
Dr. Thomas Loumeau of the Bone & Joint Institute of South Georgia, performed the first endoscopic spine surgery in the United States using the newly launched 4K Endoscopic Spine Surgery System from joimax, Inc. The surgery was performed at the Surgery Center of BJI, LLC, located in Jesup, GA. Endoscopic Spine Surgery is a state-of-the-art surgical procedure that uses micro incisions to allow your surgeon to visualize the surgical field through the use of an HD Endoscope. The procedure is performed with minimal trauma to surrounding tissues, allowing patients to get back to work and life more quickly.
Our innovative 4K endoscopic system puts BJISG on the leading edge of spine surgery offering many benefits to patients such as:
- Reduced Post-Operative Pain
- Less Blood Loss
- Faster Recovery Time
- Minimal Trauma to Surrounding Tissues
- Preserves Spine Mobility
- Less Scarring
- Less Anesthesia During Surgery
ANATOMY OF THE SPINE
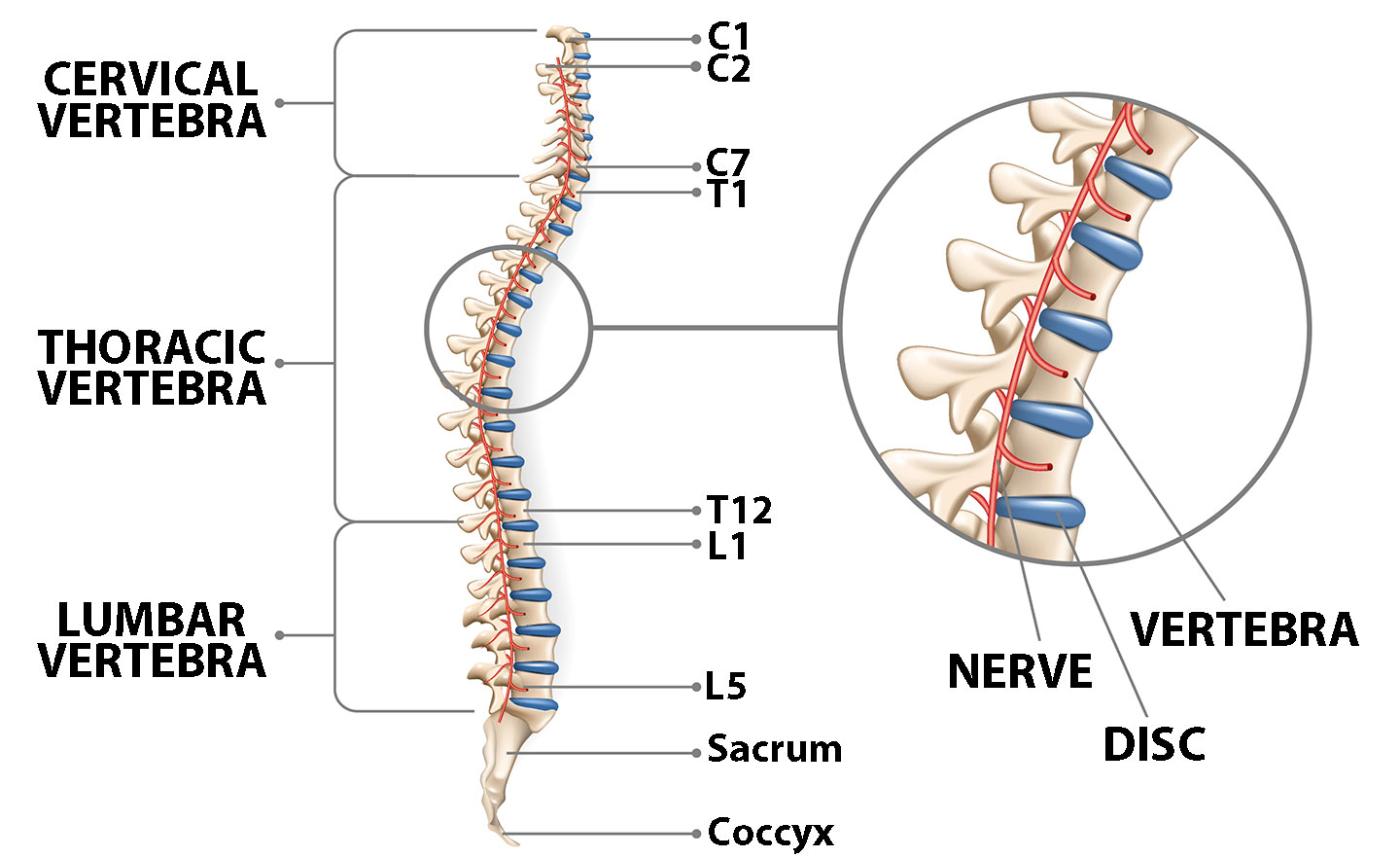
The normal anatomy of the spine is usually described by dividing up the spine into three major sections: the cervical, the thoracic, and the lumbar spine. Below the lumbar spine is a bone called the sacrum, which is part of the pelvis, and then the end of the spine, the coccyx. Each section is made up of individual bones, called vertebrae. There are 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae.
An individual vertebra is made up of several parts including the primary area of the weight-bearing body of the vertebra, the fibrous discs which separate each of the vertebrae and the lamina which covers the spinal canal (which the spinal nerves pass through).
The vertebrae are separated by intervertebral discs, which act as cushions between the bones.
Each disc, which separates the vertebrae, is made up of two parts: The hard, tough outer layer (annulus), and the center which is soft. When a disc herniates or ruptures, the soft interior of the disc escapes through a tear in the annulus and can compress a nerve root.
Spine Surgery Patients – Their Testimonies…
Watch This Video and Learn More About Thomas P. Loumeau, MD
Am I a candidate for spine surgery?
At BJISG, Surgery is always considered to be the last resort. Typically, many non-operative treatments are available depending on the diagnosis. If, however, these treatments are not effective and you and your physician decide to proceed with surgery, BJISG is equipped with the latest, state-of-the-art equipment and knowledge to proceed with a surgical option. Many spine surgeries are performed endoscopically, a very minimally invasive procedure. All surgeries are individualized to the patient and their needs for the best possible outcome.
If you are ready to find relief from your neck or back pain, request a consultation today.
SPINE SURGERY – SURGICAL PROCESS EXPLAINED:
- Diabetics – Make sure your blood sugar control is extremely good in the weeks prior to your procedure. We will check your levels the morning prior to surgery and it must be less than 120. If not, your surgery will likely be postponed.
- Smoking – If you are a smoker, we insist that you stop smoking at least 1 month prior to your surgery and continue to not smoke after surgery as this will help the healing process. You must stop smoking!
 Obesity – Being severely overweight can impact your healing negatively. We require that surgical patients have a BMI score of no more than 35 (Click here for additional information on body mass index and the weight loss diet).
Obesity – Being severely overweight can impact your healing negatively. We require that surgical patients have a BMI score of no more than 35 (Click here for additional information on body mass index and the weight loss diet).- Nourishment – It is vital that you take care of yourself and eat a healthy diet consisting of plenty of vegetables (green and other colored) and proteins (eggs, bacon, beef, pork, poultry, fish (no batter please). Cut out all unnecessary sugars and starches (the “white stuff” such as bread, rice, grits, potatoes, corn, chips, sodas and junk food in general). Try to eat well-balanced meals to give your body the nutrition it needs to heal.
- Skin – It is important to take care of your skin in the weeks prior to surgery! No bug bites, scratches, infected lacerations, etc – these allow additional places for germs to hide.
- Dental – Make sure your dental health is good – no abscessed teeth/infections, etc.
- Toe & Fingernail health – This must be excellent. No draining, bleeding, inflamed, infected or ingrown nails.
- Narcotic Pain Medications – Discontinue these medications if at all possible.
PLAN FOR YOUR SURGERY: BEFORE AND AFTER!
Make sure to plan for the fact that you are having surgery.
- Designate a close friend or family member as your “Patient Champion”
- As a patient champion, this person will be responsible to help you throughout the process of your surgery. Your patient champion will have the following responsibilities:
- Attend your Pre-Op appointment with you.
- Bring you to the facility on the day of surgery.
- Drive you home and help you into your residence.
- As a patient champion, this person will be responsible to help you throughout the process of your surgery. Your patient champion will have the following responsibilities:
- Make sure you have friends and family lined up to help you during the healing process.
- Make sure there are no trip hazards at your home.
- You will be given a prescription for pain medications before surgery – make sure someone can get it for you and stores it securely.
- Become an active member in your recovery process.
- You can do this! Your determination to succeed is critical!
STEP 2 Getting Started – Final Office Visit With Your Surgeon
- Patient Champion – Make sure to bring your patient champion with you if at all possible.
- Laboratory Screen – Blood work will be drawn or reviewed.
- Surgical Clearance – If needed, we will obtain or review a surgical clearance from your primary care physician and/or specialist (cardiologist, pulmonologist, neurologist, etc).
- Questions – Final questions and plans discussed with your surgeon.
STEP 3 Pre-Op Packet Pick-Up From BJISG
Patients will come by BJISG at an appointed time and pick up their surgical Packet which will include the following:
- Post-Op Pain Medication Narcotic Agreement
- Post-Op Prescriptions
- DME Prescription
- Post-Surgery Outpatient Physical Therapy Prescription
- Diabetic Pre-Op Instructions (for diabetics)
- Discharge Instructions
- Surgery Check follow-up appointment
STEP 4 Pre-Op Appointment
Your pre-op appointment will be held at the surgical facility.
- Patient Champion – Make sure to bring your patient champion with you if at all possible.
- Pre-Surgery Testing – Additional blood will be drawn for labs and an EKG will be taken.
- Final Surgery Consult – final details will be discussed prior to surgery. We will explain what and when to stop taking medications at this point and which need to be continued.
- Prescription Drugs – Discontinuing prescriptions that “thin” the blood as directed by your physician(s), such as aspirin is necessary prior to surgery. Any Narcotic/Opioid medications must be stopped prior to surgery as well.
- Food/Drink – Patients must refrain from eating or drinking as directed at the pre-op appointment. Make sure that you are well nourished and hydrated in the days and weeks prior to surgery (Water, Gatorade, etc).
STEP 5 Day Of Surgery
Here is what to expect the day of your surgery:
 Arrive at the surgical facility at the appointed time (with your patient champion).
Arrive at the surgical facility at the appointed time (with your patient champion).- Final pre-surgery assessment of vital signs and general health
- Diabetics – blood sugar checked and must be below 120.
- Meet with anesthesiologist and operating room nurse.
- Start IV (intravenous) catheter for administration of fluids and antibiotics.
- Your surgeon will see you, answer any last questions and “sign your surgical site”.
- Spine surgery.
- Recovery room.
- Ongoing monitoring of vital signs until condition is stabilized.
- Diet of clear liquids or soft foods, as tolerated.
- Begin post-op activities taught during the pre-op visit.
STEP 6 Going Home
Typically, patients who undergo Spine Surgery may require a hospital stay but some patients can go home the same day as their surgery. Each patient recovers differently but all must reach the following goals before being discharged home:
- Vital signs stable (Blood pressure, heart rate, temperature, respiration)
- Ability to get from the bed to the bathroom and back to the bed with or without a walker.
- Ability to walk 50 feet down the hall and back.
- Ability to urinate and have a bowel movement.
- Nausea and/or vomiting controlled.
- No medication interactions or adverse side effects.
- Ability to tolerate eating and drinking.
- Pain reasonably controlled with Oral Medications.
- Diabetic patients must have their blood sugars well controlled.
If you are released the same day, your patient champion will drive you home and help you into your house.
You will be given specific DISCHARGE INSTRUCTIONS and AT HOME EXERCISES for your care/recovery after you leave the surgical facility.
SPECIALIZED SPINE PROCEDURES OFFERED:
Endoscopic Spine Surgery
Endoscopic Spine Surgery is a state-of-the-art minimally invasive surgical procedure that uses micro incisions to allow the surgeon to visualize the surgical field through the use of a High Definition Endoscope. The procedure is performed with minimal trauma to surrounding tissues, allowing patients to get back to work and life more quickly.
Benefits include:
- Reduced Post-Operative Pain
- Preserves Spine Mobility
- Less Blood Loss
- Less Scarring
- Faster Recovery Time
- Less Anesthesia During Surgery
Transforamenal Lumber Interbody Fusion (TLIF)
Spinal Osteotomy
Spinal Instrumentation
Scoliosis Correction
Posterior Lumbar Inverbody Fusion (PLIF)
Minimally Invasive Spine Surgery
Microdescectomy
Laminotomy
Laminoplasty
Laminectomy
Kyphoplasty
Foraminotomy / Foraminectomy
Direct Lateral Interbody Fusion
Cervical Disc Replacement
Anterior Lumbar Interbody Fusion (ALIF)
Anterior Cervical Discectomy & Fusion (ACDF)


